
Greeting from Professor

Mutsumi Okazaki, M.D., Ph.D.
Professor and Chairperson, Department of Plastic and Reconstructive Surgery, Graduate School of Medicine, The University of Tokyo.
Profile
1990 Graduated from The University of Tokyo, School of Medicine.
2000 Chief, Department of Plastic Surgery, Asahi General Hospital.
2002 Assistant professor, Department of Plastic and Reconstructive Surgery, The University of Tokyo Hospital.
2006 Associate professor, Department of Plastic Surgery, Kyorin University.
2009 Professor and Chairperson, Department of Plastic and Reconstructive Surgery, Graduate School of Science, Tokyo Medical and Dental University.
2017 Professor and Chairperson, Department of Plastic and Reconstructive Surgery, Graduate School of Medicine, The University of Tokyo.
International Associate Editor, Plastic and Reconstructive Surgery ® (2019-2022)
International Associate Editor, PRS Global Open (2015-2020).
Field of expertise
- Reconstruction of facial deformity and dysfunction
- Reanimation for facial paralysis
- Microsurgery
Reanimation for Facial Paralysis
At Plastic and Reconstructive Surgery in The University of Tokyo Hospital, we perform surgical operations that are highly satisfying for patients using our ideas and ingenious and dexterous techniques, and had published the achievements obtained for the benefit of the world. Here we present our surgical treatments of facial nerve paralysis
1. Reconstructive operations around the eyes using eyeblink evaluation as an indicator A patient with facial nerve paralysis suffers in two ways: eyelid opening difficulty occurs due to upper eyelid ptosis caused by frontalis muscle paralysis, and eyelid closure disorder also results from orbicularis oculi muscle paralysis. Regarding eyelid closure disorder, until now, the ability to intentionally close the eyelid has been used as an indicator.
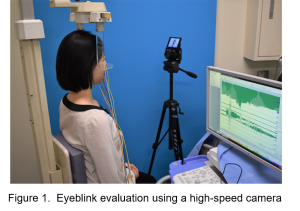
However, symptoms that trouble patients are related to eyeblink, such as corneal inflammation and dryness or pain in the eyes. Therefore, in 2016, our division introduced an eyeblink evaluation using a high-speed camera. An eyeblink test is conducted on patients with facial nerve paralysis, with several tens of thousands of frames analyzed with each test. Based on the analysis results, a reconstructive procedure for the area around the eyes that best suits each patient is determined, as well as the appropriate amount of correction (Figure 1).
2. Reconstruction of laughing and eyelid closing functions using multi-split vascularized nerve and muscle
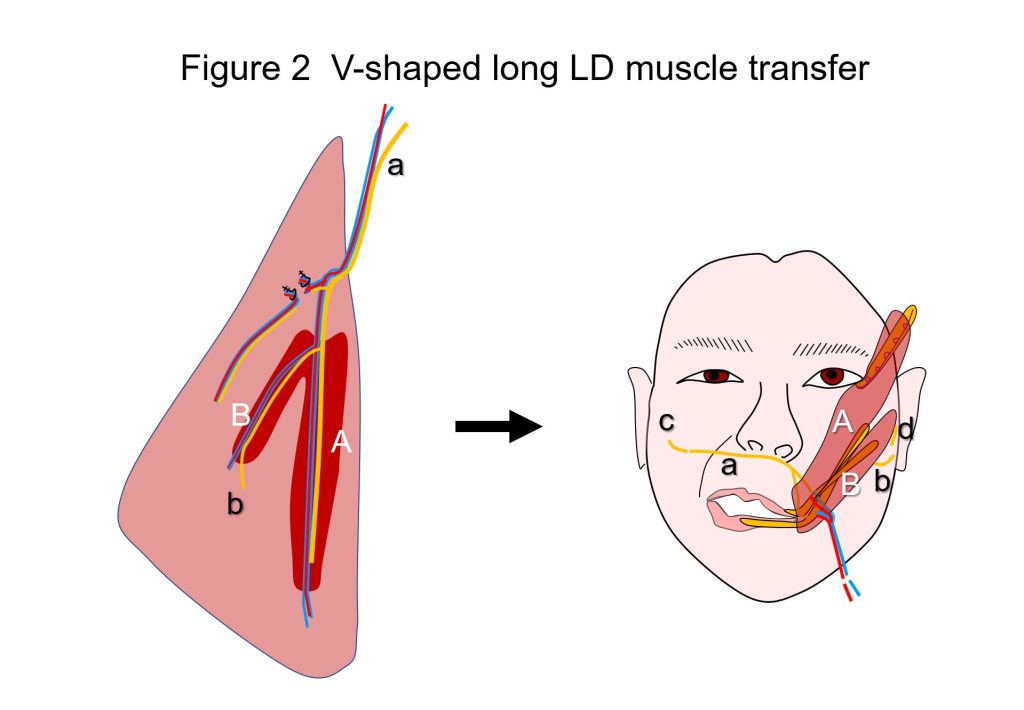
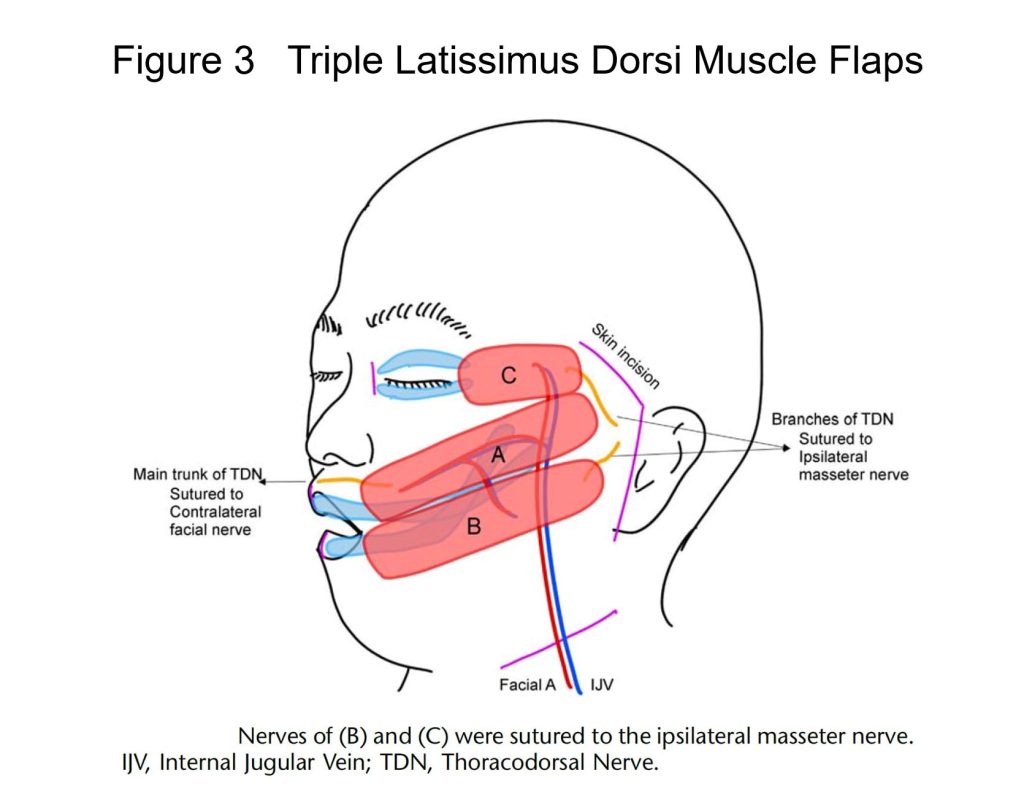
Patients with facial nerve paralysis tend to avoid laughing as much as possible because facial asymmetry becomes conspicuous when laughing due to the mouth being pulled to the opposite side, caused by impaired muscle movement involved in the process. From the viewpoint of QOL, restoring the ability of patients to laugh by reconstructing movement affected by paralysis is a highly significant achievement. Nerve and muscle transplantation has been conducted using microscopic microvascular anastomosis. As the power source for muscle power movement, either 1) a facial nerve on the opposite side or 2) the masseteric nerve on the same side has been used. While 1) has the benefit of enabling unintentional spontaneous laughing, movement was occasionally weak. Similarly, while 2) enabled intentional and strong movement, unintentional spontaneous laughing is difficult, and therefore patients had to artificially make laughing motions through initiating biting movement. The technique required for 2) is easier, making this procedure still the more popular choice in many countries, particularly Europe and the U.S. The procedure for 1), which is more difficult, is performed at five to ten facilities across Japan. Both 1) and 2) have their respective strengths and weaknesses, with the selection for one or the other largely depending on the skill level of the surgeon. We had devised and published a hybrid method that splits into two a single muscle supplied by a pair of artery and vein, and sutures the nerve of the respective muscle to the facial nerve of the healthy side and to the masseter nerve of the affected side in 20152). This method combines the strengths of both procedures above, enabling the patient both to laugh spontaneously as well as artificially, with a level of surgical intervention that is mostly equivalent to 1) or 2). And recently, we developed the revised version1) of our previous method2). It is the hybrid of single innervated muscle transfer and dually innervated muscle transfer. The largest characteristics of this procedure is that the V-shaped long latissimus dorsi muscle offers eye smiling (upward movement of the lower eyelid, with bulging of the malar region, during smiling) (Figure 2). This smiling eye atmosphere in sync with spontaneous peri-oral smiling gives an expression of real spontaneous smiling to everyone. We have also devised a procedure that further advances the technique above by splitting the muscle into three, and transplanting them while suturing the respective nerves to different nerves, thereby achieving intentional eyelid closing function in addition to the voluntary and spontaneous smile3) (Figure 3).
3. More complex reconstruction of facial features and functional disorders
Major deformation of the face may result in patients with bone or soft tissue defects in addition to facial nerve paralysis, due to tumor resection or traumatic injury. For such patients, we perform surgery to transplant vascularized bones and adipose tissue at the same time as muscle4) (Figure 4). Simultaneous implementation of such a complex procedure reduces the required number of surgical operation sessions, thereby relieving burden to the patient, and also supporting faster rehabilitation.
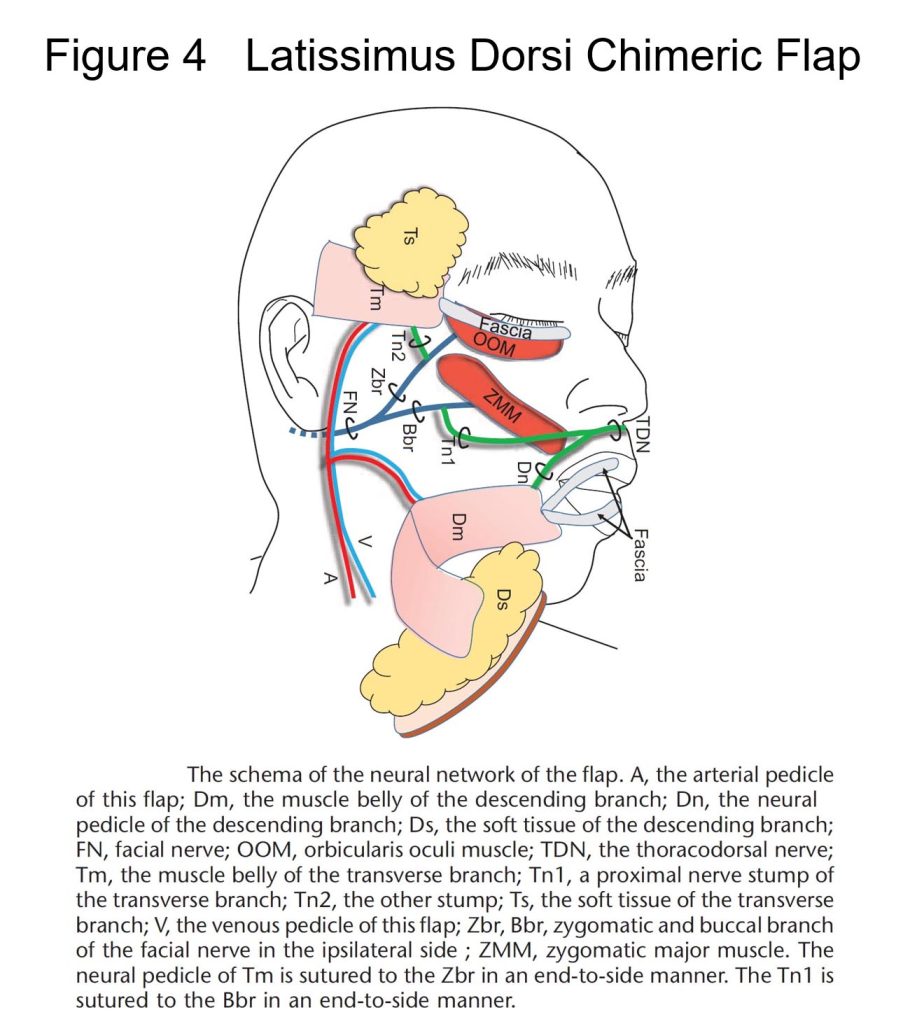
Figure 4. Free dual LD muscle transfer combined with dual adipose flaps (reference 3).
4. Treatment of viral facial nerve palsy sequelae
Viruses make up a large share with regard to the causes of facial nerve palsy. Owing to multidisciplinary drug treatment in Otorhinolaryngology, severe sequelae have become rarer in recent years. However, it is easy to imagine the extreme stress to patients resulting from sequelae to the face, as it is one of the most conspicuous parts of the body. Typical sequelae include: weak facial movement even though the face is pulled relatively strongly while the affected side is at rest (contracture type); synkinetic movement that is different from that intended (the corner of the mouth is pulled sideways, even though the patient wants to close his/her eyelid; the eye closes when the patient moves his/her mouth: synkinesis); and a drooping eyebrow resulting in a drooping eyelid that hinders the patient’s vision despite the patient being mostly recovered. We provide tailor-made treatments for each patient while listening to their complaints. At The University of Tokyo Hospital, a cooperative structure has been established with the Otorhinolaryngology Department. Once otorhinolaryngologic treatment has been completed, the patient is transferred to Reconstructive Surgery. We support enhanced QOL of patients by seamlessly taking over the treatment process, even if sequelae endure. If you are seeking medical advice concerning facial deformation or movement disorder (facial nerve palsy): See the details regarding symptoms and treatment by visiting https://www.h.u-tokyo.ac.jp/english/centers-services/clinical-divisions/plastic/index.html. Requests for consultation and inquiries concerning hospital visits from patients with facial nerve palsy are accepted at the e-mail address below:
utokyoprs.counsel@gmail.com
★ Free Neuromuscular Transfer for Facial Reanimation
1) Okazaki M, Miyamoto S, Tomioka Y, Fujisawa K. Simultaneous reconstruction of smiling eye using V-shaped long latissimus dorsi muscle transfer in patients with flaccid facial paralysis. Plast Reconstr Surg. 2024 Oct 1;154(4):873-878.
2) Okazaki M, Tanaka K, Uemura N, Usami S, Homma T, Okubo A, Hamanaga M, Mori H. One-stage dual latissimus dorsi Muscle flap transfer with a pair of vascular anastomoses and double nerve suturing for long-standing facial paralysis. J Plast Reconstr Aesthet Surg. 2015; 68: e113-9.
3) Matsusaka R, Okazaki M, Tanaka K, Uemura N, Mori H, Homma T, Kanayama K.
Simultaneous reconstruction of voluntary and spontaneous smiles and eyelid closure with triple latissimus dorsi muscle flaps. J Craniofac Surg. 2024 Oct 31. Online ahead of print.
4) Umemoto N, Okazaki M, Tanaka K, Miyamoto S, Iida T. Long-term follow-up of secondary reconstruction of facial paralysis and depressive deformities after subtotal temporal bone resection. J Craniofac Surg. 2024 Oct 7. Online ahead of print.
5) Homma T, Okazaki M, Tanaka K, Uemura N. Simultaneous surgical treatment for smile dysfunction and lagophthalmos involving a dual latissimus dorsi flap. Plast Reconstr Surg Glob Open. 25; 5: e1370, 2017.
6) Ogawa K, Okazaki M, Tanaka K, Uemura N, Homma T. One-stage simultaneous augmentation of 2 regions of 3 facial reanimations after mid skull base surgery by using a neurovascular latissimus dorsi chimeric flap. J Craniofac Surg. 2021; 730-733.
7) Ogawa K, Okazaki M, Tanaka K, Uemura N, Homma T. Chimeric latissimus dorsi flap in one-stage reconstruction of depressor muscle dysfunction and depression deformity in the perimandibular area. J Craniofac Surg. 2021; 32(7): 2512-2515.
★ Blink and Movement Analysis
8) Ogawa K, Okazaki M, Mori H, Hidaka T, Tomioka Y, Tanaka K, Uemura N, Akiyama M. Comparative blink analysis in patients with established facial paralysis using high-speed video analysis. J Craniofac Surg. 2022;33(3):797-802.
9) Hidaka T, Ogawa K, Tomioka Y, Yoshii K, Okazaki M. The Impact of brow-lift on eyelid closure in patients with facial paralysis Facial Plast Surg Aesthet Med. 2022 Sep-Oct;24(5):385-390.
10) Hidaka T, Ogawa K, Tomioka Y, Yoshii K, Tomio J, Okazaki M. Change in eyelid closure in spontaneous blinking after static eyelid reconstruction surgery for patients with facial paralysis. Ann Plast Surg. 2022 Mar 1;88(3):303-307.
11) Hidaka T, Kurita M, Ogawa K, Tomioka Y, Okazaki M. Application of artificial intelligence for real-time facial asymmetry analysis. Plast Reconstr Surg. 2020 Aug;146(2):243e-245e.
★ Other publications concerning the treatments for facial paralysis
12) Tomioka Y, Okazaki M, Matsutani H, Ohba J, Miyakuni A. Dual-plane lift-and-hold technique for brow ptosis in young patients with facial paralysis.J Plast Reconstr Aesthet Surg. 2024 Jun;93:203-209.
13) Hidaka T, Miyamoto S, Ogawa K, Tomioka Y, Okazaki M. Factors associated with late admission to facial plastic surgery among patients with long-standing facial paralysis. Ann Plast Surg. 2021 Nov 1;87(5):547-551.
14) Tanaka K, Suesada N, Homma T, Mori H, Tsutsumi T, Asakage T, Okazaki M. Muscle-penetration method: Cable nerve grafting with well vascularized surrounding tissue and shortest graft length. J Plast Reconstr Aesthet Surg. 2022 Apr 27:S1748-6815(22)00238-8.
15) Homma T, Uemura N, Tanaka K, Mori H, Okazaki M. Objective assessment of the repeated botox treatment to the synkinesis of facial paralysis by the integrated electromyography. J Craniofac Surg. 2024. Online ahead of print.
16) Tomioka Y, Okazaki M, Matsutani H, Ohba J, Miyakuni A.
Dual-plane lift-and-hold technique for brow ptosis in young patients with facial paralysis.
J Plast Reconstr Aesthet Surg. 2024; 93: 203-209.
17) Tanaka K, Okazaki M, Yano T, Miyashita H, Homma T, Tomita M. Quantitative evaluation of blood perfusion to nerves included in the anterolateral thigh flap using indocyanine green fluorescence angiography: a different contrast pattern between the vastus lateralis motor nerve and femoral cutaneous nerve. J Reconstr Microsurg. 2015; 31: 163-70.
★ Selected publications concerning reconstructions of facial deformities
Tomioka Y, Okazaki M, Matsutani H. Frontalis suspension through infrabrow skin excision for blepharoptosis in Asians. Plast Reconstr Surg. 2024 Nov 1;154(5):1015e-1019e.
Tomioka Y, Okazaki M, Kurita M, Fujisawa K, Matsutani H. Stair-step incision for composite grafts in nasal reconstruction. J Craniofac Surg. 2023 Nov-Dec 01;34(8):2464-2467.
Hidaka T, Tanaka K, Minami M, Mori H, Okazaki M. Risk factors for postoperative infection after maxillary reconstruction using skeletal grafts. J Craniofac Surg. 2023; 34: e649-e651.
Numahata T, Kitamura Y, Okazaki M. Successful repair of a forehead depression deformation due to En Coup de Sabre using costal cartilage transplantation. J Craniofac Surg. 2022; 33: e585-e586.
Tanaka K, Suesada N, Homma T, Mori H, Okazaki M. Reliability of temporal vascular anastomosis and techniques for better outcomes. J Reconstr Microsurg. 2022;38:41-46.
Kitamura Y, Oki M, Kurita M, Okazaki M. Combined use of an innervated radial forearm flap and labia minora peripheral skin graft for total upper lip reconstruction. J Craniofac Surg. 2020:1678-1680.
Higashino T, Okazaki M, Mori H, Yamaguchi K, Akita K. Microanatomy of sensory nerves in the upper eyelid: A cadaveric anatomical study. Plast Reconstr Surg. 2018.142: 345-353.
Tanaka K, Okazaki M, Homma T, Yano T, Mori H. Bilateral inferior alveolar nerve reconstruction with a vascularized sural nerve graft included in a free fibular osteocutaneous flap after segmental mandibulectomy. Head & Neck. 2016; 38: e111-4.
Usami S, Okazaki M, Tanaka K, Homma T, Yano T. Lengthening the pedicle of a scapular osseous free flap by angular branch reconnection within the subscapular artery system.
Microsurgery. 2014; 32: 662-665.
Okazaki M, Tanaka K, Kodaira S, Homma S, Miyashita H. One stage transfer of 2 paddles of thoracodorsal artery perforator flap with 1 pair of vascular anastomoses for Barraquer-Simons syndrome. J Craniofac Surg. 2012; 23 : 883-5.
Okazaki M, Ueda K, Sasaki K, Shiraishi T, Kurita M, Harii K. Expanded narrow subcutaneous-pedicled island forehead flap for reconstruction of the forehead. Ann Plast Surg, 2009; 63: 167-70.
Okazaki M, Hisatomi T, Sarukawa S. Aesthetic upper lip reconstruction with vermilion submucosal-pedicle cross-lip flap. J Craniofac Surg. 2006; 17: 1259-1262.
Okazaki M, Sarukawa S, Fukuda N. A patient with congenital defect of nasal cartilaginous septal and vomeral bone reconstructed with costal cartilaginous graft. J Craniofac Surg. 2005; 16: 819-822.
Okazaki M, Ueda K. The long Abbe flap combined with periosteally-vascularized mandibular bone for the simultaneous reconstruction of upper lip and supportive columella. Sc J Plast Reconstr Surg Hand Surg 2003; 37: 296-299.









